The logic of the market does not make it possible to improve healthcare for all. When profit and savings take precedence, respect for decent working conditions and quality of care decline..
Austerity and commercialisation: a tragedy for staff
One way of making savings in the healthcare sector is to reduce spending on health and safety at work. The COVID-19 pandemic painfully demonstrated this. Although carers work in dangerous conditions, they are not provided with sufficient protective equipment. The shortage of masks, hydro-alcoholic gel and gloves has left staff particularly vulnerable to infection. According to the WHO, by May 2021, around 115,000 carers worldwide had succumbed to COVID-19 after one year of the pandemic.

Higher workload
Healthcare workers around the world are making their voices heard. They are frustrated by their working conditions and the way in which they have to do their jobs. The pandemic has caused many people to leave the healthcare sector. As a result, the work now relies on far fewer workers.. The workload is enormous and the profession requires more and more staff. Cheaper, more flexible, more efficient. Time management and paperwork are favoured at the expense of quality care.
This can also be seen in nursing homes, especially when private players are managing care. There's no time to talk to patients, everything is ordered down to the minute. The quality of care declines and care staff no longer find their work satisfying. Stress, physical problems and burnout are the inevitable consequences.. Prolonged absences of members of staff logically increase the workload of their colleagues.
Less safety at work
During the pandemic, health workers were applauded in abundance. But today, there is still no real support. Working conditions for healthcare staff remain highly questionable, especially in the private sector. A study of healthcare workers in Catalonia shows that nurses in the private sector are more likely to work for lower wages and irregular hours than those in the public sector. This has a considerable impact on their mental and physical health. In addition, temporary work is on the increase worldwide. It is becoming increasingly difficult to obtain a permanent contract. For example, in India's booming private sector, permanent contracts are rare.

As a result, healthcare staff are often paid less, or just above the minimum wage. Sometimes, private sector pay packages are more attractive than those in the public sector, but precarious contracts mean that staff accumulate fewer pension, sick leave or unemployment rights. Moreover, overtime is not always paid and the risk of unjustified dismissal is very high.
Weaker unions
Together, we're stronger! That's what unions are all about: bringing together healthcare workers and acting with one voice. They are the lever that makes it possible to tackle unhealthy working conditions in a targeted way.. Unions negotiate better pay conditions, denounce the lack of flexibility and ensure that staff rights are respected. However, in the private sector, the number of unionised care workers is much lower. In Poland, for example, there are barely 5 %.
Everywhere, care workers are even losing their jobs for joining a union. And some private health companies are doing everything they can to prevent the formation of unions.. This phenomenon is called union busting and runs counter to Article 23 of the Universal Declaration of Human Rights (UDHR): everyone has the right to form and/or join a trade union.
| LET'S TAKE A LEAF OUT OF THE UK'S BOOK «Understaffing costs lives!” This message has resounded repeatedly in the UK since December 2022. For the first time, tens of thousands of nurses demonstrated. Through this historic strike, they called for the strengthening of the NHS, the British national health service. At the same time, on 10 January 2023, the UK Conservative government decided to submit a controversial Strike Bill to Parliament. This bill allowed the government and employers to require care workers to provide a minimum service in the event of a strike. The bill applied in particular to the health and education sectors.. Yet it was precisely these sectors that took to the streets in large numbers in the months leading up to the government's announcement. The bill allowed employers to make it easier to dismiss striking workers and take trade unions to court. A slap in the face for British public sector staff, who see strike action as their last resort in the face of the unbearable cost of living in the UK. |
Brain drain
And finally.., outsourcing healthcare to commercial investors is detrimental to the public sector, as it diverts scarce resources such as qualified professionals. One example is the way in which the presence of the for-profit private sector in one country, or the medical tourism industries in neighbouring countries, lure health professionals away from the public sector by offering them higher salaries. This «brain drain» or «care drain», both internal and international, leads to a shortage of healthcare staff in the public sector and in rural areas. The result is a lack of access to quality healthcare for a large proportion of the population.
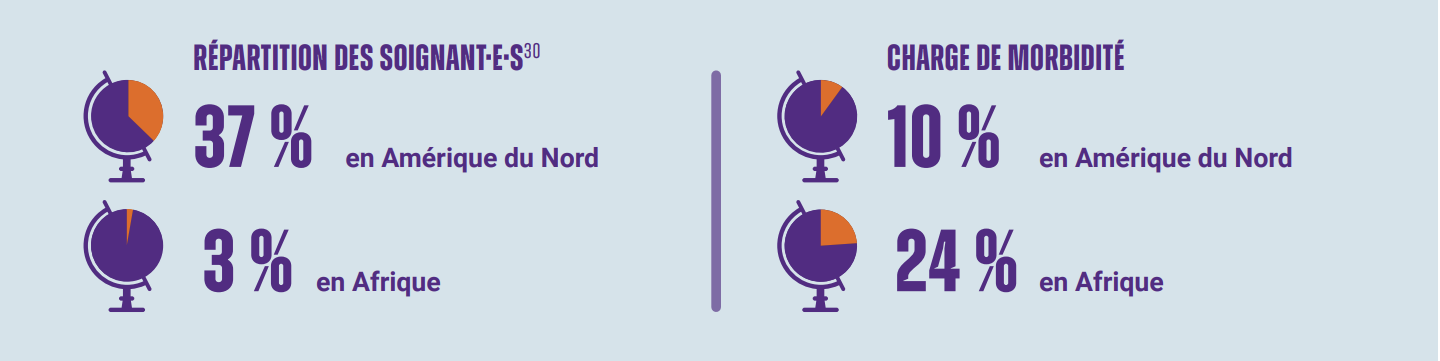
Low-income countries are particularly hard hit. They are seeing a large number of their health professionals emigrate to high-income countries, which are trying to solve their own shortages by creating new ones elsewhere. Low-income countries bear the cost of training healthcare workers, while high-income countries reap the benefits. The International Organisation for Migration estimates that low-income countries lose 500 million dollars a year due to the migration of healthcare professionals to high-income countries.
Big Pharma's thirst for profit versus healthcare professionals
Big pharma has made colossal profits in recent years. In 2022, Pfizer will have earned 100 billion dollars. A record. As much as the total health expenditure of 100 countries combined. Yet the COVID-19 vaccination campaign can hardly be described as a success.
Especially for healthcare professionals in low-income countries. By the end of 2021, after one year of vaccination, barely one in three carers had been vaccinated. This is despite the fact that healthcare workers have been identified as a priority group for vaccination against COVID. Big Pharma's thirst for profit is killing healthcare workers.
